
Varicose Veins
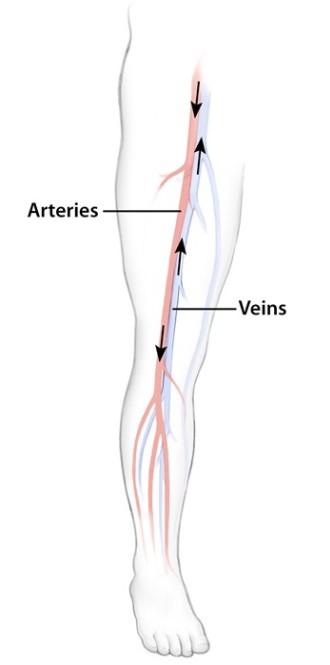
The heart pumps blood to supply oxygen and nutrients to all parts of the body.
- Arteries carry blood from the heart towards the body parts, while veins carry blood from the body parts back to the heart.
- As the blood is pumped back to the heart from the legs, one-way valves in the veins prevent the blood from flowing backward, which would happen because of the pull of gravity when a person is standing.
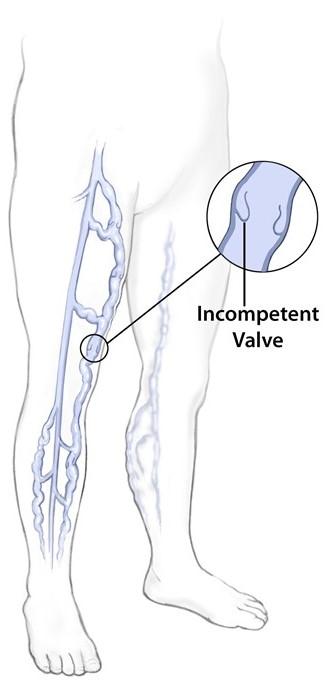
- If a one-way valve becomes weak, some of the blood can leak back into the vein, collect there, and then become congested or clogged.
- This congestion will cause the vein to abnormally enlarge.
- These enlarged veins can be either varicose veins or spider veins.
Varicose veins are very swollen and raised above the surface of the skin. They are dark purple or blue in color and can look like cords or very twisted and bulging. They are found most often on the backs of the calves or on the inside of the leg, anywhere from the groin to the ankle.
Causes and Symptoms
The saphenous vein extends from the groin along a medial path down the inner side of the thigh and leg down to the ankle. Varicose veins are clusters of dilated or enlarged veins attached to the main saphenous vein that occur when the valves in the veins malfunction. Veins can lose elasticity with age, causing them to stretch out. When that happens, blood that should be moving toward the heart may flow backward. Blood pools in the veins, causing them to enlarge and become varicose. The exact cause of spider and varicose veins are unknown, but there are several factors that can cause a person to be more likely to develop them:
- Heredity - being born with weak vein valves
- Hormonal changes that occur during puberty, pregnancy, and menopause, as well as taking estrogen, progesterone, and birth control pills
- Aging
- Obesity
- Leg injury
- Prolonged standing, such as for long hours on the job
You may have symptoms even before varicose veins appear. Signs and symptoms may include:
- Dilated veins along the upper or lower leg
- Distended and tender veins which cause leg fatigue
- Phlebitis (inflammation) which causes pain, tenderness, and redness along the enlarged segment of the varicose vein
- Ulcerations of the skin overlying the varicose veins, which can lead to infection
On rare occasions, phlebitis within large varicose veins can extend into the deeper veins of the leg and lead to dangerous blood clots in the lung, called pulmonary embolism.
Treatment
All treatment options should be thoroughly discussed with a doctor. Depending on the severity of the symptoms, treatment can involve:
- Simply doing nothing - if there are no symptoms or pain.
- Wearing firm-fitting elastic stockings
- Sclerotherapy - injecting a solution into the vein that causes the lining of the vein walls to swell, stick together, and eventually seal shut stopping the flow of blood and turning the vein into scar tissue. In a few weeks, the vein should fade. Although the same vein may need to be injected with the solution more than once, sclerotherapy is very effective if done correctly. Sclerotherapy does not require anesthesia and can be done in the doctor's office.
- Electrodesiccation - similar to sclerotherapy except the veins are sealed off with an electrical current instead of the injection of solution. This treatment may leave scars.
- Endovenous Ablation - placing a special catheter or a very small tube into the vein sending radiofrequency or laser energy to cause the vein wall to shrink and seal shut. Healthier veins surrounding the closed vein restore the normal flow of blood allowing the varicose vein to decrease. This is a noninvasive procedure and can be done in a doctor's office. The only side effect is slight bruising.
- Surgical Ligation and Stripping - tying the veins shut and completely removing them from the leg. Removing the veins will not affect the circulation of blood in the leg because veins deeper in the leg take care of the larger volumes of blood. This surgery requires either local or general anesthesia and must be done in an operating room usually on an outpatient basis.
- Transilluminated Powered Phlebectomy - is a clinically tested surgical technique for varicose vein removal. “Transilluminated” refers to the passing of light under the skin and “phlebectomy” is the medical term for vein removal. In this procedure, the surgeon removes the vein using a small powered surgical device while viewing the vein using a transilluminating light. Clinical studies suggest that this method enables the surgeon to remove veins using a minimal number of small incisions and short operative times, which may result in an easier recovery for the patient with good cosmetic results. 1,2
- Ambulatory Phlebectomy - a light source marks the location of the vein where tiny incisions are made. With surgical hooks, the vein is pulled out of the leg. This surgery requires local or regional anesthesia. The vein usually is removed in one treatment. The most common side effect is slight bruising. Patients can return to normal activity the day after treatment.
Questions to Ask the Doctor
- What is the worst thing that can happen if I do nothing?
- I have heard of treatment requiring no incisions. What are the advantages and disadvantages of laser or radiofrequency treatment?
- Does it hurt to inject the varicose veins with sclerosing solutions?
- Is it dangerous?
- How effective is it?
- Can the varicose veins come back?
- Do the solutions cause any pigment problems in the skin?
- I have heard that stripping the entire saphenous vein gets rid of the problem completely. Is this true?
- Can the varicose veins come back?
- Are there any side effects to stripping the entire saphenous vein?
- What type of specialist is best qualified to deal with varicose veins: a general surgeon, vascular surgeon, plastic/cosmetic surgeon, or dermatologist?
If there is any doubt, please seek a second and a third opinion. The more these options are discussed with a doctor, the easier it will be to determine the best course of treatment for each individual condition.
1 Franz RW, Knapp ED. Annals of Vasc Surg. 2008; 23(3):303-309.
2 Passman M. Vascular. 2007; 15:262-268.