
Blood Clots
Thrombi (clots) are masses that form within the circulatory system on the inside of arteries, the heart, and prosthetic (artificial) surfaces such as catheters and stents. They are composed of elements of the clotting system, white blood cells (fight infection), and red blood cells. Thrombus formation is a process involving many factors that interact with each other. Although the formation of thrombi may occur as part of a natural "healing" process, inside the arterial system their course is unpredictable and they can cause serious problems.
Indeed, acute arterial thromboembolism is a serious medical problem. It is characterized by sudden occlusion of an artery supplying blood to tissues of the body, resulting in loss of function or tissue death if it is not treated immediately or does not resolve spontaneously. Although acute thromboembolism can affect the upper extremities, the vessels supplying the head and brain, and even arteries leading to internal organs, it occurs more commonly in the lower extremities (legs and feet).
Arterial thromboembolism is usually caused by one of the following:
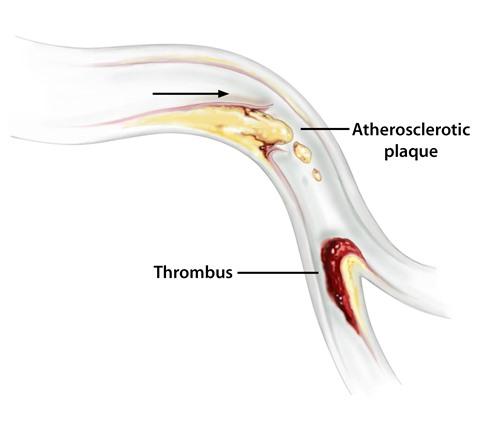
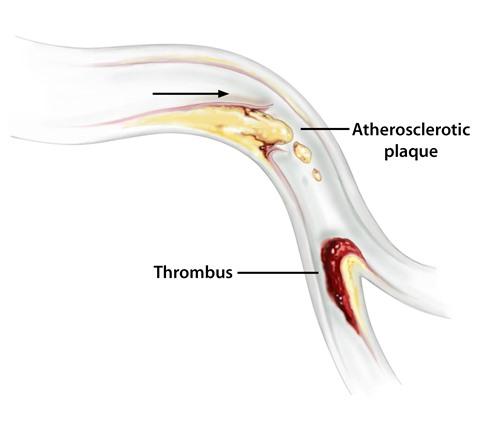
- Ruptured atherosclerotic plaque above the region that becomes occluded
- Acute thrombosis (clotting) on top of existing atherosclerotic disease
- An embolism from the heart, aorta, or other large vessel that breaks off and travels to a vessel "downstream" and lodges
- A dissecting aneurysm (tear in the wall of a major artery that may rupture and spill blood outside the artery)
Arterial thromboembolism is a significant cause of death and disability in the United States. It is a serious problem partly because it is usually the result of a dangerous underlying disease, and also because it often occurs suddenly and without warning. Acute arterial thromboembolism usually occurs at locations where the inner wall of a blood vessel has been damaged or where there is disturbance or change in the pattern of blood flow.
From an anatomical standpoint, acute occlusions typically occur at branch points in an artery. A small area of plaque forms on the inner wall of an artery at the point where the artery splits or branches into two tributaries. This occurs at this location because of:
- The turbulence of the blood flow at this point
- Subsequent damage of the inner layer of the arterial wall
- Increased incorporation of LDL cholesterol and other components into the damaged area
- Deposition of cholesterol and components of the clotting system
Pieces of the plaque can break off and float downstream or a clot may form on the top of the plaque and break off later.
Risk Factors
Although there are other causes, most patients have underlying atherosclerosis, one of the most important contributing factors to arterial thromboembolism. The major risk factors for atherosclerosis include those listed below. Although each of these factors is important alone, they can also be additive if they occur together:
- Hypertension
- Elevated levels of low density lipoprotein
- Reduced levels of high density lipoprotein
- Cigarette smoking
- Diabetes mellitus
- Obesity
- Male gender
- Elevated homocysteine levels
- Family history of premature atherosclerosis
Diseases of the peripheral arteries, such as acute thromboembolism, increase in frequency with age.
Signs and Symptoms
Clinical manifestations of arterial occlusion depend on the vessel involved, the extent of obstruction, how rapidly occlusion progresses, and whether collateral flow is adequate. However, for patients with an acute arterial thromboembolism, the history usually includes:
- Sudden onset of severe pain
- Coldness, numbness, and pallor (paleness) in the affected extremity
- Loss of pulse beyond the site of the obstruction in the occluded artery
Deciding About Treatment
In the past, direct surgical intervention was the only feasible alternative. More recently non-invasive techniques have been developed. When the issue of treatment is being considered, it is important to ask as many questions as possible before the patient and doctor together decide on the optimal treatment. If a patient does not feel comfortable with his or her understanding of the treatment options, it is wise to get a second or third opinion. So what are the options?
Types of Therapy
Many newer treatments for vascular disease, such as an arterial occlusion, avoid open surgery. These treatments may be performed by interventional radiologists, vascular surgeons, or cardiologists.
- PTA: The primary approach is percutaneous transluminal angioplasty (PTA), whereby a small high-pressure balloon is used to open an obstructed vessel. However, because of the high recurrence rate of obstruction, alternative methods may be necessary.
- Stent placement: Stents (metallic meshlike tubes) are often inserted into the vessel at the site of the obstruction. Stents are very strong and may keep the vessel open much better than balloons alone. Moreover, the recurrence rate is reportedly less. Stents work best in large arteries with high flow.
- Thrombolytic therapy: Thrombolytic therapy involves the infusion of drugs to unclog the artery (break up the clot). This approach, especially by regional catheter infusion, is most effective for acute arterial occlusions of less than two weeks duration.
- Embolectomy: The purpose of this procedure is to remove a localized clot in an artery. An incision is made in the skin over the artery and the artery exposed. A small incision is made in the artery and a small balloon tipped catheter is inserted. The catheter is pushed pass the clot, the balloon inflated and the catheter removed dragging the clot with it.
- Endarterectomy: An incision is made in the skin over the vessel that is blocked with plaque. An incision along the length of the artery is made in the arterial wall and the plaque is peeled out of the artery and the incision closed with or without a patch. The patch is made of a section of vein or an artificial material.
- Bypass graft: A bypass graft channels blood around a block in an artery. This may be done in combination with one of the other procedures.
Questions for the Doctor
Here are some questions patients should ask the doctor. In some cases, the answers are dependent on the treatment:
- What is the advantage of using clot-busting drugs (or stents or immediate surgery)?
- If the drugs don't work, have we lost time?
- Have we increased the chances that surgery will fail and I will lose my leg?
- How long will you try the less invasive methods before recommending surgery?
- Are there any complications to the use of drugs, such as bleeding?
- If I prefer surgery, what are the pros and cons?
- What treatment would you choose and why?
- How many cases have you performed of this type?
- What are your results?