
Aortic Aneurysms
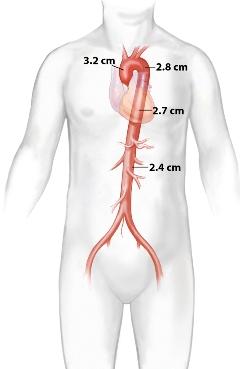
The aorta is the largest artery in the human body. It originates from the left ventricle in the heart, and traverses the chest (thoracic aorta), and the abdomen (abdominal aorta) where it splits (divides) into the iliac arteries destined to become the leg arteries lower down. The aorta gives off arterial branches that bring blood supply and oxygen to all organs and tissues: brain, liver, kidneys, and everything else - including the heart muscle itself! The diameter or size of the normal aorta is an important reference point. These are the average measurements that are expected for older adults with a height between 5'6" and 5'10":
- 3.2 cm in the ascending aorta and proximal arch
- 2.8 cm in the proximal descending
- 2.7 cm in the mid descending
- 2.6 cm in the distal descending thoracic aorta
- 2.3-2.5 cm in the infrarenal abdominal aorta
It is important to note that 0.6 cm should be added or subtracted from these figures for adults more than 6 feet or less than 5 feet in height.
An 'aneurysm' forms when the aortic wall bulges out (balloons) as a result of a focal or segmental weakening related to loss of its elastic tissue. As such, it is thought of as a 'degenerative disease' - and degenerative is in fact the correct modern-day designation for most of these aneurysms. It tends to affect individuals of a certain age, over 50 years of age in the vast majority. Men are affected far more frequently than women.
The likelihood of developing an aortic aneurysm is related to a number of risk factors. These are the most significant:
- heredity (genes, family history of aortic aneurysms)
- smoking
- chronic obstructive pulmonary disease (COPD)
- coronary and atherosclerotic peripheral arterial disease (PAD)
Unquestionably, the most important risk factor is by far the history of a blood relative (parent, sibling) having had an aortic aneurysm. This, in and of itself, should prompt the consideration of screening to rule out the presence of an aortic aneurysm. The two most commonly used diagnostic studies performed for such screening are an abdominal (aortic) ultrasound, and a CT scan of the entire aorta. The latter may be favored since it has the ability to image the entire aorta and uncover both thoracic and abdominal aneurysms, whereas ultrasound is only effective in the diagnosis of an abdominal aneurysm.
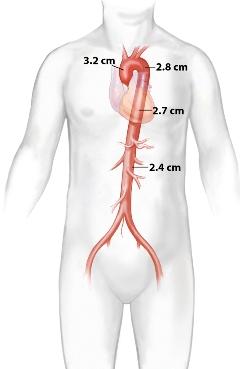
Anatomically, aneurysms are generally classified as fusiform (or 'concentric') when the disease involves the entire circumference of the vessel, or saccular (or 'eccentric') when the sac affects only a portion of the circumference. The latter is generally considered to be more dangerous because of their propensity to rupture (burst), but fusiform aneurysms are far more common. Once developed, the natural history of an aortic aneurysm is one of continued growth and eventual rupture. The latter is often fatal. On the average, aneurysms grow about 0.4 cm per year. 'Rapid growth' is defined as an enlargement more than twice that much, usually 1cm or more in 6 months' time. The larger the aneurysm the more likely it is to rupture. "Significant" or "dangerous" aneurysms are those that have already reached a size of >5.0 cm in maximum diameter.
Treatment ('repair') is aimed at preventing death from aneurysm rupture. These are the generally accepted indications for repair of an AAA at the present time:
- AAA 5.5 cm or larger for males
- AAA 5.0 cm or larger for females
- AAA with recent rapid growth (enlargement)
- Strong family history of AAA rupture
- Patients' wishes
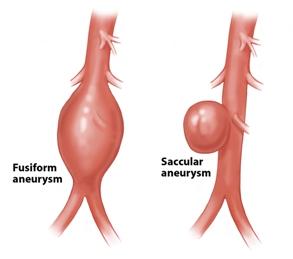
The surgical approach was developed in the 1950s and 60s and has evolved considerably since then. It involves the performance of a major intra-abdominal (or intra-thoracic) operation and cross-clamping of the aorta, with aneurysm repair done by means of segmental replacement of the diseased segment of the aorta with a straight tube or bifurcated vascular graft. It is an important and frequently performed vascular surgical operation and one that tends to produce good long-term results. However, it does carry considerable risks because of its invasive nature and high morbidity with frequent major complications. Patient recovery also is an issue as it can be prolonged and difficult. Operative mortality (at 30 days), while reasonably low (1-5%), is also significant.
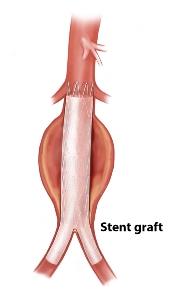
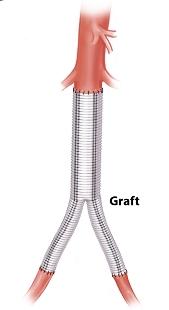
The less-invasive endovascular approach was developed in the 1990s. It relies on the placement of an endoluminal stent-graft device that excludes (isolates) the aneurysm sac from pressure and flow. Often, the aneurysm shrinks afterward, and occasionally 'resolves' or virtually disappears. The procedure involves 1 (or 2) small incision in the groin and avoids a major intra-abdominal or intra-thoracic operation altogether. Some operators perform it using a totally percutaneous approach ("key-hole" surgery).
Endovascular repair is generally preferred but only when the anatomy of the aorta and aneurysm are suitable for such an approach. The advantages are clear: less invasive, fewer complications, a short hospitalization, and a quick and simple recovery. However, it is important to understand that disadvantages exist as well, such as the need for close surveillance and monitoring over time, involving usually a CT scan study done yearly or more frequently; the need for re-intervention; and lingering uncertainties about long-term results.
Traditional open surgery, on the other hand, is a well-established and proven treatment approach that has been performed for decades. It can be used virtually in every case, but patients with significant co-existing medical conditions (co-morbidities) face a higher risk of complications, sometimes serious or even fatal. Hospitalization is considerably longer, as is the recovery and its complexity. Long-term results of the conventional open surgical approach tend to be excellent, but patients still need to be followed and monitored over time.